On December 1, 2023, North Carolina will become the 40th state to implement Medicaid expansion under the Affordable Care Act (ACA), extending Medicaid eligibility to more than 600,000 adults with incomes up to 138% of the federal poverty level (FPL).
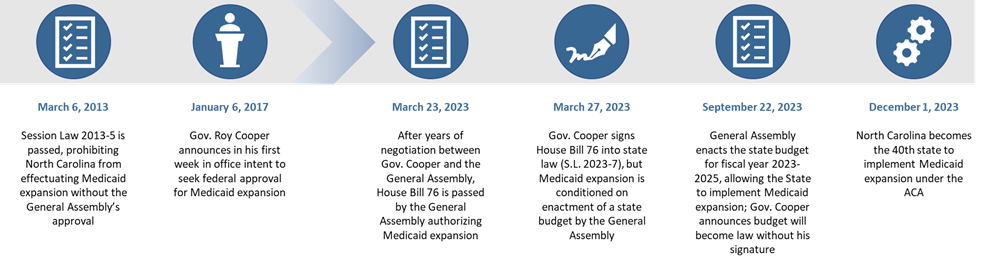
North Carolina’s path to Medicaid expansion has spanned more than a decade. Shortly after the 2012 National Federation of Independent Business v. Sebelius U.S. Supreme Court ruling made Medicaid expansion optional, North Carolina’s General Assembly passed Session Law (S.L.) 2013-5 prohibiting North Carolina from effectuating Medicaid expansion without the General Assembly’s approval. Governor Roy Cooper (D) has pursued expansion since he entered office in January 2017, but year after year, the proposal failed to receive sufficient support in the General Assembly.
Over the past two years, several shifts in the federal and State landscape helped reset the terms of the discussion. First, financing for expansion became even more favorable. The 2021 American Rescue Plan Act (ARPA) provided an eight quarter, five percentage point increase in the regular federal medical assistance percentage for states that newly adopted Medicaid expansion after March 11, 2021. This is in addition to the enhanced 90% federal matching rate for expansion populations provided in the ACA. For North Carolina, the enhanced funding under ARPA translated into an additional $1.8 billion. The State also developed a new strategy for financing the non-federal share of expansion through the State’s hospitals, avoiding the need for Medicaid expansion to compete with other items in the State’s general funds. North Carolina also has made substantial changes to transform the delivery of healthcare services under Medicaid, including transitioning from a predominantly fee-for-service Medicaid program to Medicaid managed care, a change mandated by the General Assembly. Finally, as evidence has continued to mount on the health and economic benefits of Medicaid expansion, polling has shown strong support for expansion among North Carolina voters. Ultimately, North Carolina Senate President Pro Tempore Phil Berger (R), once a staunch opponent of expansion, concluded, “Medicaid expansion if implemented in a reasonable, responsible manner is a positive for state fiscal and healthcare policy.”
On March 23, 2023, North Carolina’s General Assembly passed House Bill 76 authorizing Medicaid expansion (“NC Health Works”), which was signed into law by Governor Cooper as S.L. 2023-7 shortly thereafter. But still, there was a catch: the law made expansion contingent on the passage of the State’s budget. After months of negotiations, on September 22, 2023, the General Assembly passed the State’s 2023-2025 biennium budget. That same day, while voicing strong opposition to items in the budget unrelated to expansion, Governor Cooper announced his intention to allow the budget to become law without his signature to permit Medicaid expansion to take effect without further delay.
North Carolina’s expansion will be effective on December 1, 2023, giving the State an important new opportunity to retain coverage gains from the continuous coverage guarantee during the COVID-19 Public Health Emergency.1 North Carolina is currently processing more than 2.9 million redeterminations after a three-year pause. To date, North Carolina has renewed coverage for 79% of enrollees, the fourth highest rate of renewals among states—a figure that seems poised to grow with Medicaid expansion.
Graphic 1: North Carolina’s Timeline to Medicaid Expansion
Key Features of Legislation
In addition to authorizing expansion, S.L. 2023-7 establishes new Medicaid payments to hospitals, a workforce development program, certificate of need reforms, and funding to support Medicaid eligibility determinations, among other provisions. Concurrently, the budget allocates approximately $700 million of the $1.8 billion that the State expects to receive through the ARPA enhanced match to strengthen North Carolina's mental health and substance use disorder (SUD) delivery system. Key provisions of both pieces of legislation are described below.
S.L. 2023-7 Enabling Medicaid Expansion
Financing Sources for NC Health Works. Under the ACA, the federal government covers 90% of the cost of coverage for expansion adults, and states are required to cover the remaining 10%, referred to as the non-federal share. Under S.L. 2023-7, expansion will not require any increase in State General Fund spending. The non-federal share of expansion costs will be financed in full using the following sources:
- A new tax on acute care hospitals;
- Increased intergovernmental transfers (IGTs) from public hospitals to the State; and
- Premium taxes assessed on Medicaid managed care plans for expansion enrollees.
Sunset Clause for Expansion. The legislation includes a “sunset provision” that would terminate coverage for the expansion group if: (1) the federal share of expansion costs drops below 90%, or (2) if the 10% non-federal share cannot be fully financed through the sources described above.
Medicaid Work Requirements, Pending Indication of Federal Approval. S.L. 2023-7 requires that “if there is any indication” the federal government will resume authorizing work requirements as a condition of Medicaid eligibility, North Carolina’s Department of Health and Human Services (DHHS) must apply and negotiate for federal approval to implement them. The Biden Administration has taken the position that conditioning Medicaid eligibility on work requirements does not further the objectives of the Medicaid program—a reversal from the Trump Administration.
Workforce Development Program. By December 1, 2024, North Carolina’s Department of Commerce must submit a plan to the legislature for a statewide workforce development program that coordinates workforce development efforts across State agencies, including DHHS. Among other requirements, S.L. 2023-7 requires DHHS to coordinate with the Department of Commerce to develop strategies to connect individuals newly enrolled in Medicaid and other social service programs to the workforce development program, including by linking them to a workforce development case manager. The Department of Commerce and DHHS are required to report to the legislature every five years on Medicaid enrollees’ participation in workforce development programs and relevant outcomes (e.g., wage increases, ineligibility for Medicaid due to employment).
Creation of Healthcare Access and Stabilization Program (HASP). DHHS is required to request federal approval to establish HASP, a state-directed payment program that would increase Medicaid reimbursement to acute care hospitals and critical access hospitals up to levels comparable to reimbursement from private health insurers. Under HASP, the State will make quarterly payments to Medicaid managed care plans covering the difference between Medicaid base rates and a payment level that more closely reflects commercial payment rates. Managed care plans will in turn distribute directed payments to hospitals in their networks. Payments will be financed entirely using funds collected through quarterly assessments on acute care hospitals, IGTs from public hospitals and federal funds. The legislation provides detailed methodology by which DHHS must calculate the hospital assessments and IGTs that will finance the HASP payments.
Certificate of Need Reforms. S.L. 2023-7 includes changes that exempt certain facilities and expenditures, such as licensed home care agencies providing Early and Periodic Screening, Diagnostic, and Treatment services, increases in chemical dependency treatment and psychiatric beds at existing facilities and purchases of replacement medical equipment, from requiring DHHS’ “certificate of need” review and approval process.
Support for Medicaid Eligibility Determinations. DHHS will provide $4 million in funding to County Departments of Social Services (County DSS) to support eligibility determinations for individuals newly eligible for Medicaid due to expansion. Additionally, S.L. 2023-7 temporarily permits, for up to 12 months, the Federally Facilitated Marketplace to conduct Medicaid eligibility determinations to further reduce administrative burden on County DSS.
New Initiatives Funded Under State Budget by ARPA Enhanced Match
The 2023-2025 fiscal biennium budget also allocates approximately $700 million in funding generated by the ARPA enhanced match to support the State’s mental health and SUD delivery system. These investments include rate increases to mental health and substance use providers, in addition to investments such as:
- $99 million for community-based behavioral health programs for justice-involved populations.
- $80 million to support community-based and other specialized treatment options for children and families with significant behavioral health and other complex needs.
- $10 million for recruitment and retention of behavioral health providers working in outpatient primary care settings in rural, underserved areas of the State.
- $40 million for sign-on and retention bonuses to members of the behavioral health workforce at state healthcare facilities including psychiatric hospitals, developmental centers, alcohol and drug treatment centers, neuro-medical treatment centers and residential programs for children.
Moving Forward
With expansion and the significant new investments in its healthcare and social service system financed by the ARPA enhanced federal matching funds, North Carolina is undertaking a once-in-a-generation effort to improve the health of its residents. North Carolina joins six other states in implementing Medicaid expansion since 2020: Utah, Idaho and Nebraska in 2020; Oklahoma and Missouri in 2021; and South Dakota thus far in 2023. While these other states have pursued Medicaid expansion through voter support on ballot initiatives, North Carolina’s expansion of Medicaid through the legislative process is notable for its bipartisan support. The Kaiser Family Foundation estimates that if the remaining ten states2 adopted Medicaid expansion, approximately 3.5 million individuals would newly gain coverage. For these states, the ARPA enhanced match remains available as an additional incentive to implement Medicaid expansion.
1 The 2020 Families First Coronavirus Response Act required states to main continuous coverage of nearly all enrollees as a condition of accessing enhanced federal Medicaid funding during the COVID-19 Public Health Emergency. Over the past several months, states have resumed Medicaid redeterminations.
2 Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin and Wyoming.