The Big Picture
In recognition of the impact of health-related social needs (HRSNs),1,2 the Centers for Medicare & Medicaid Services (CMS) issued a new Informational Bulletin and accompanying framework on November 16, which together outline coverage options for housing and nutrition services under Medicaid. The new guidance reiterates the importance of addressing HRSNs to improved health and summarizes (and in some cases updates) multiple previous sources of CMS guidance on HRSN coverage under Medicaid and Children’s Health Insurance Program (CHIP) authorities.
Broadly, the bulletin sheds new light on key features of HRSN services that CMS considers “allowable.” Specifically, the guidance for the first time comprehensively articulates the following:
- A list of 15 HRSN services that CMS will approve.
- Details on which Medicaid authorities may be used to authorize each HRSN service (1115 waivers, in lieu of services (ILOS), home and community-based services (HCBS) waivers, state plan amendments, and CHIP health services initiatives).
- Specific guardrails on eligible populations and durational limits on service by authority.
Summary of HRSN Bulletin and Framework
Allowable Services and Authorities
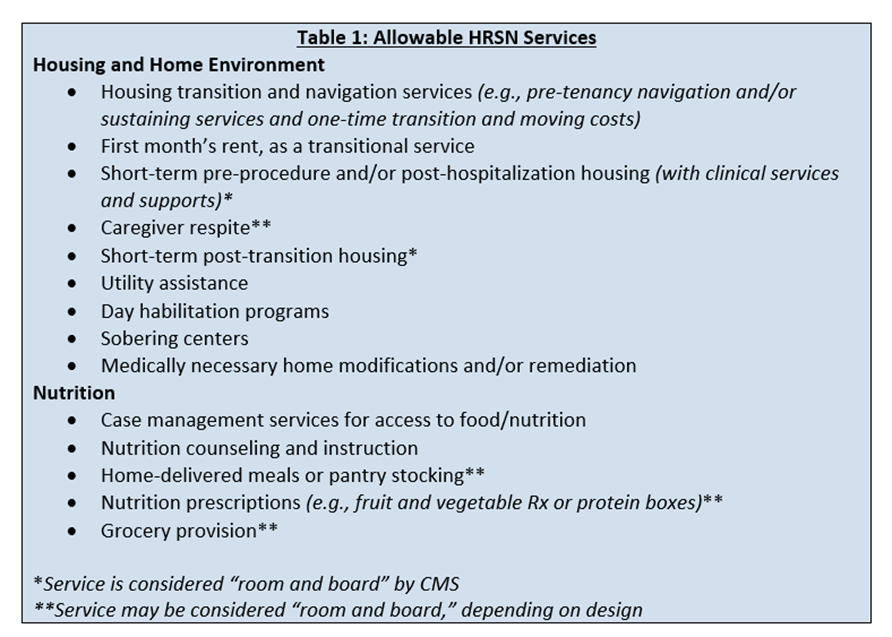
For the first time, this guidance provides a list of 15 HRSN services CMS considers “approvable.” The services span two major domains: 1) housing/home environment and 2) nutrition (see Table 1). The guidance is silent on whether or under what circumstances other domains or services could also be approvable.
Most services can be authorized under multiple authorities. Consistent with recent 1115 waiver approvals in multiple states, the guidance indicates that 1115 waiver authority can be used to authorize a number of services that CMS considers to be “room and board,” departing from long-standing prohibitions in Medicaid on the use of federal matching dollars to pay for such services. These services, which include temporary housing, utility assistance, and nutrition services covering three meals per day, can only be authorized under 1115 waivers and come with new limitations on eligible populations and duration, reviewed below.
Durational and Eligibility Limits on ‘Room and Board’ Services
The guidance also clarifies expectations on durational limits for services. Services that include room and board are generally time-limited to a period of six months:
- Utility assistance and short-term housing may only be provided for six months and once per demonstration period.
- Nutrition supports that provide three meals per day are limited to six months but may be renewed for additional six-month periods if the enrollee continues to meet eligibility criteria.
Housing services that include room and board are limited to use by populations experiencing housing or care transitions, such as individuals who are homeless or are transitioning from an institution into the community. CMS does not impose any new eligible population or duration limits on services that are not considered to be “room and board,” including services like housing navigation, nutrition education/counseling, or nutrition supports provided for less than three meals a day.
Other Eligibility Criteria for HRSN Services
For all HRSN services, states must propose “clinically focused, needs-based criteria” to define who is eligible to receive the particular HRSN service. CMS provides examples of allowable population types, which can include children and pregnant individuals identified as high risk, individuals who are homeless or are at risk of becoming homeless, individuals with serious mental illness and/or substance use disorder, and individuals experiencing high-risk care transitions. Certain services and authorities are further limited to specific high-needs populations, including, for example, the following:
- Some HCBS authorities are limited to individuals who meet institutional levels of care.
- Temporary housing and utility assistance are limited to individuals who are experiencing life transitions—including, for example, individuals who are transitioning out of a justice-involved setting, are transitioning out of the child welfare system, or are considered homeless or at risk of homelessness.
- Grocery provisions are limited to “high-risk individuals to avoid unnecessary acute care admission or institutionalization.”
Financing Requirements
CMS has imposed certain requirements on how states finance HRSN services. These requirements vary by the authority type. States opting to use 1115 waivers to cover the costs of HRSN services must abide by explicit spending limits set by CMS. Specifically, states may not spend more than three percent of their total computable Medicaid spending on HRSN and are subject to provider rate increases. ILOS must be deemed cost-effective by the state and are subject to different spending limits. Specifically, expected ILOS costs must be less than five percent of managed care capitation in any given managed care delivery system. (See CMS guidance on use of ILOS.)
Enrollee Protections
CMS emphasizes existing regulatory protections for enrollees and clarifies that existing rights and protections for Medicaid managed care enrollees apply to enrollees receiving HRSN services, including rights to file appeals and grievances, to fair hearings, and to receive information on available treatment options and alternatives. Further, the guidance is clear that states and/or managed care plans may not require an enrollee to utilize HRSN services or reduce, discourage, or jeopardize enrollee access to state plan services or settings based on whether an enrollee opts to receive HRSN services.
Looking Ahead
By codifying guidance related to HRSN, CMS is expanding the tools available to states to creatively address nonmedical needs of Medicaid members that negatively impact health. At the same time, the new guidance leaves many questions unanswered. Most notably, it is unclear whether or under what standards CMS will consider approving HRSN services that are not listed among the 15. Services not on the list that have previously been approved under prior administrations or under HCBS authority include those that address transportation, interpersonal violence, and employment needs of Medicaid enrollees. Further, the eligibility guidance for most services remains high-level (those who meet “clinically focused, needs-based criteria”), with a fairly narrow list of examples, raising questions about the level of discretion CMS will grant states in defining eligibility criteria. As CMS responds to the multiple states with pending HRSN service requests in the coming months, their intentions on these and other questions are likely to become clearer.
1 Robert Wood Johnson Foundation. Medicaid’s Role in Addressing Social Determinants of Health. February 1, 2019.
2 De Salvo, Karen and Leavitt, Michael. For an Option to Address Social Determinants of Health, Look to Medicaid. Health Affairs. July 8, 2019.